Recent advancements in speed and accuracy of 3D printing technologies have allowed surgeons to simulate procedures using life-size anatomical models that are created directly from a patient’s CT scan or MRI. The team at Dinsmore recently completed a patient-specific project with the Children’s Hospital of Orange County (CHOC).
Eighteen-year old Moises Campos had a tibial tubercle fracture from a previous injury that left him with a growth arrest below his kneecap and a deformity of the tibia. The deformity affected his ability to walk and run, and put him in danger of early onset arthritis. The only way to correct this was to cut the bone and slowly move it back to the correct position.
Dr. Afshin Aminian, medical director, CHOC Children’s Orthopedic Institute and the pediatric orthopedic surgeon assigned to Moises’s case, contacted the Dinsmore team to work with him and his team on a 3D model of the tibia prior to surgery. The complex nature of Moises’s bone deformity could make intra-operative assessment difficult. Creating a customized 3D model of the deformed bone would allow the surgery team to see, study, and plan for deviations from typical anatomy, taking much of the guesswork out of the operation.
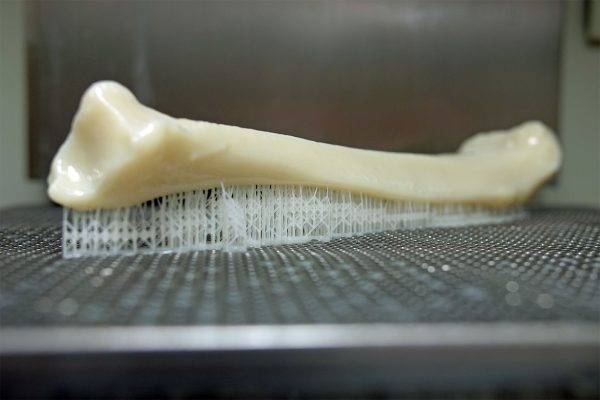
Using CT scan data provided by the hospital, Dinsmore’s in-house designers converted the data of bone anatomy into a surface model from which they 3D printed a model of the bone. Jay Dinsmore, President and Founder of Dinsmore Inc. described the engagement and project with the CHOC surgeons as something his team was very proud to support.
“We were excited to take on this project and hopefully have a positive impact on Moises’ surgery. We printed several models with the data from a series of CT scans over a few weeks. The front-end work of ensuring data integrity was the most time-intensive step of the process, but also the most important. At Dinsmore, we are proud to offer our customers design for prototyping as a service to ensure that their data and files are prepared appropriately for guaranteed successful prints.”
The Dinsmore team used a 3D printing technology called stereolithography (SLA) to produce the model– a process that is frequently chosen for both its precision and speed. To achieve the most realistic aesthetic results, Dinsmore’s team took a unique approach to the process and only partially cured the resin while post-processing to produce a density and surface finish that more closely resembled bone.
With the newly printed model in hand, Dr. Aminian’s team planned their cuts and fitted the bone with the appropriate external fixation construct. As Dr. Justin Roth, a surgical team member said, “for complex surgeries like this one, the 3D physical model was a great conceptual practice tool for pre-surgical planning. It gave us a tactical visualization of the deformity so we could get a better sense of what needed to be done to correct it. You can measure the deformity in CT scans, but there’s nothing like being able to hold the physical model.”
This advanced planning makes for smoother and more effective execution during the operation, leading to a better outcome for the patient. Dr. Roth also noted the value of having the model in hand to educate the patient and family about the procedure. “It’s nice to be able to take the model and show patients what’s going to happen during surgery.” he says.
The collaboration between the surgeons at CHOC and the team at Dinsmore produced a successful surgery that restored Moises’ normal gait and function in just 4 four months. In six months, Moises returned to his normal activities without any restrictions. His stepmother explained her excitement for his recovery, saying that “the surgery has had a genuine impact on his life. He is more confident in his interactions with other children and is excited to participate in activities that he used to avoid. We are so thankful for the surgical team at CHOC.”